Chapter 13
Heart and Circulation
Lub-dub, lub-dub, lub-dub! Seventy beats each minute, 4,200 beats each hour, 100,800 beats each day your heart contracts, ejecting blood into elastic blood vessels for distribution around the body. Blood is mostly water and proteins, with millions of red blood cells (erythrocytes) carrying oxygen, white blood cells (leukocytes) defending against infections, and platelets (thrombocytes) plugging vascular leaks. Platelets are intimately involved in blood clotting, or coagulation — a rapid series of complex positive feedback events that serve to stop bleeding. With the bleeding stopped, the disturbance has been corrected (negative feedback) and homeostasis has been restored.
The heart has blood receiving chambers (atria) and blood pumping chambers (ventricles) with valves at each exit to ensure the continuous flow of blood. Each complete cardiac cycle starts with a spontaneous electrical excitation followed shortly by a mechanical contraction of the myocardium. The electrical cycle originates from the pacemaker region and spreads throughout the heart, as recorded on the electrocardiogram (ECG). In this manner, both normal and abnormal (arrhythmia) cardiac cycles can be evaluated. Potential life-threatening interruption in blood flow to the myocardium (ischemia) is one example of cardiac conditions that reveals itself on the ECG. The mechanical cycle is characterized by pressure and volume changes within the heart that result in the ejection of blood and the formation of two valve sounds (lub-dub) that can be heard with a stethoscope.
Blood is forced out of the heart and into large arteries, which branch into smaller and smaller arterioles. Beyond arterioles, miles of capillaries cruising close to all living cells are active in the exchange of gases and nutrients for wastes. After this exchange, blood is drained away from tissue capillaries through venules and then larger veins, returning to the heart for another boost around the vascular network.
Since some fluid and other materials are forced out of capillaries, and others are released from neighboring cells, the lymph system vessels (lymphatics) provide a beautifully designed drainage system for the filtering and recycling of extracellular fluid that eventually returns to the blood. In the next chapter, the focus is on the arterioles, where blood pressure and the distribution of blood flow to various parts of the body such as the kidney, skin, and brain is regulated. These two chapters combine to provide a circulatory theme that helps us to better understand the following chapters that discuss the respiratory (chapter 15), urinary (chapter 16), digestive (chapters 17 and 18), and endocrine (chapters 11 and 20) systems.
Blood serves numerous functions, including the transport of respiratory gases, nutritive molecules, metabolic wastes, and hormones. Blood is transported through the body in a system of vessels leading from and returning to the heart.
a. glucose.
b. Na+.
c. K+.
d. albumin.
e. Ca2+.
47. You are a red blood cell entering the heart from the superior vena cava! Test your understanding of cardiac structures by tracing your route through the entire heart, past the valves, and into the aorta. Starting with number 1, write the numerical sequence of the following structures on the left in the spaces provided. On the right side of the page, write out the name of the structure that corresponds to the numerical sequence from 1 to 12 that you have chosen. The last one, number 12 (aorta), has been done for you. Notice that the pulmonary circulation is included. Completion of figure 13.1 should be of further help in learning these structures.
Notice that the pulmonary circulation is included. Now label the figure in the next section.
pulmonary capillary
mitral valve
aortic semilunar valve
tricuspid valve
pulmonary vein
12 aorta
left ventricle
right ventricle
right atrium
pulmonary semilunar valve
left atrium
pulmonary artery
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12. aorta
Study figure 13.1 and label all structures of the heart, including the four valves. When finished, check your work with figure 13.11 in your text.
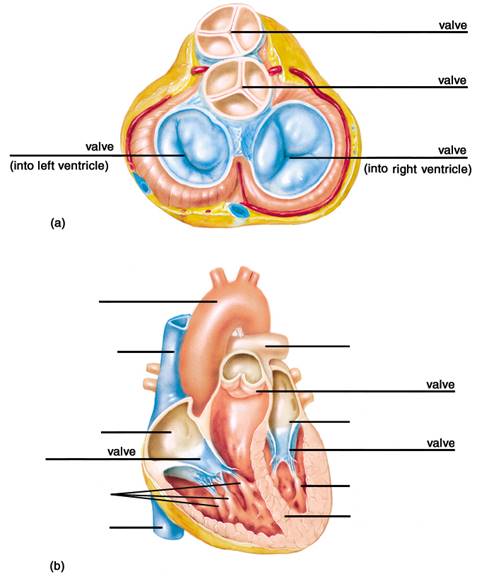
Figure 13.1
The two atria fill with blood and then contract simultaneously. This is followed by simultaneous contraction of both ventricles, which sends blood through the pulmonary and systemic circulations. Contraction of the ventricles closes the AV valves and opens the semilunar valves; relaxation of the ventricles causes the semilunar valves to close. The closing of first the AV valves and then the semilunar valves produces the “lub-dub” sounds heard with a stethoscope.
a. contraction phase and relaxation phase of the atria.
b. relaxation phase and contraction phase of the atria.
c. contraction phase and relaxation phase of the ventricles.
d. relaxation phase and contraction phase of the ventricles.
e. the simultaneous contraction and relaxation phases of both the atria and the ventricles.
a. one-fourth
b. one-third
c. one-half
d. two-thirds
e. three-fourths
a. 0.3; 0.5
b. 0.4; 0.4
c. 0.1; 0.7
d. 0.6; 0.2
e. 0.2; 0.6
a. left heart pumps a greater volume of blood than the right heart.
b. right heart contracts shortly before the left heart.
c. right heart pumps blood with less force (at lower pressure) than the left heart.
d. left heart has a shorter cardiac cycle duration than the right heart.
a. opening of the AV valves.
b. closing of the AV valves.
c. opening of the semilunar valves.
d. closing of the semilunar valves.
e. Both b and d are correct.
The pacemaker region of the heart (SA node) exhibits a spontaneous depolarization that causes action potentials, resulting in the automatic beating of the heart. Electrical impulses are conducted by myocardial cells in the atria and are transmitted to the ventricles by specialized conducting tissue. Electrocardiogram waves correspond to the electrical events in the heart as follows: P wave (depolarization of the atria); QRS wave (depolarization of the ventricles); and T wave (repolarization of the ventricles).
a. demonstrates spontaneous electrical activity.
b. depolarizes to threshold before other cardiac regions.
c. has Ca2+ diffusing through Ca2+ channels into the cardiac fibers.
d. develops pacemaker potentials during diastole.
e. All of these statements are correct.
a. slow outward diffusion of Na+.
b. fast inward diffusion of Na+.
c. fast outward diffusion of Ca2+.
d. slow inward diffusion of Ca2+.
a. Lead I is a recording from the right arm to the left arm.
b. The unipolar leads are found only on the chest.
c. There are a total of twelve standard ECG leads that “view” the changing pattern of the heart’s electrical activity.
d. There are six unipolar chest leads.
e. Lead III is a recording from the left arm to the left leg.
a. The T wave represents depolarization of the atria.
b. The QRS wave represents depolarization of the ventricles.
c. The repolarization of the atria is hidden by the QRS wave.
d. The P wave occurs shortly before the QRS wave.
e. All of these statements about the ECG are true.
a. P wave.
b. P-R interval.
c. QRS wave.
d. T wave.
e. S-T segment.
Study the drawing of the electrical conduction pathway of the heart in figure 13.2. Then write the words that best describe the conduction pathway structures indicated by the blank lines on the figure. Remember this is the pathway for electrical excitation — the mechanical contraction of cardiac muscle fibers will follow shortly. See figure 13.20 in the text to check your work.
Figure 13.2 The conduction system of the heart.
The thick muscle layer of arteries allows them to transmit blood ejected from the heart under high pressure, and the elastic recoil of the large arteries further contributes to blood flow. The thinner muscle layer of veins allows them to distend when an increased amount of blood enters them, and their one-way valves ensure that blood flows back to the heart. Capillaries are composed of only one layer of endothelium, which facilitates the rapid exchange of materials between the blood and tissue fluid.
a. externa
b. media
c. interna
d. endothelium
a. Arteries have more smooth muscle than comparable veins.
b. Arteries carry blood under higher pressure.
c. Veins have one‑way valves, promoting flow in only one direction.
d. Veins collapse thereby providing the greatest resistance to blood flow in the circulatory system.
e. All of these statements regarding arteries and veins are true.
a. arteries.
b. arterioles.
c. capillaries.
d. venules.
e. veins.
a. continuous capillary.
b. discontinuous capillary.
c. fenestrated capillary.
a. the inhalation (inspiratory) phase of normal breathing
b. large skeletal muscle contractions (pump)
c. the higher average hydrostatic pressure in the veins than that found in the heart
d. standing upright, perfectly still
Atherosclerosis is a disease process that can lead to obstruction of coronary blood flow. As a result, the electrical properties of the heart and its ability to function as a pump may be seriously compromised. Abnormal cardiac rhythms, or arrhythmias, can be detected by the abnormal electrocardiogram patterns they produce.
a. Monocytes, attracted to the tunica intima region of the damaged endothelium, engulf lipids and take on a “foamy cells” appearance.
b. Gray-white “fatty streaks” formed by lipid-filled macrophages, protrude into the lumen of arteries and thus reduce blood flow.
c. White blood cells (phagocytes) attempt to attack and reject the developing atheroma as a foreign substance.
d. Fibrous plaques may form, composed of accumulated lipids, white blood cells, and debris, covered by a cap of connective tissue and smooth muscle cells.
e. All of these events are part of the long-term progression in atherosclerosis.
a. advanced age
b. smoking
c. high blood HDL — cholesterol
d. hypertension
e. high blood LDL — cholesterol
a. In the liver, LDL consists of droplets of cholesterol, neutral fat, free fatty acids, and phospholipids surrounded by an outer layer of protein molecules.
b. LDL levels are typically higher in females and in exercising males than in those who are inactive.
c. The apolipoproteins molecules in LDLs are recognized by specific receptors located on various body cells resulting in attachment and ingestion of the LDLs by receptor-mediated endocytosis.
d. Persons with high blood LDL levels usually have a low number of LDL receptors in their livers.
e. LDL blood levels rise in persons with high cholesterol, in those eating high-fat diets, and in people with familial hypercholesteremia.
a. An MI is commonly referred to by the general public as a “heart attack.”
b. An MI may be detected by changes in the S‑T segment of the ECG.
c. Since myocardial cells are adapted to respire anaerobically for several hours, an MI takes time to develop.
d. An MI can be diagnosed by the abnormal release of creatine phosphokinase (CPK) and lactate dehydrogenase (LDH) enzymes released from the infarcted cells.
e. All of these statements regarding an MI are true.
a. flutter
b. fibrillation
c. tachycardia
d. bradycardia
e. AV node block
Lymphatic vessels absorb excess tissue fluid and transport this fluid — now called lymph — to ducts that drain into veins. Lymph nodes, and lymphoid tissue in the thymus, spleen, and tonsils produce lymphocytes, which are white blood cells involved in immunity.
This essay tutorial will answer the first essay question found in the “Review Activities” section of your Human Physiology textbook. Please read Essay Question 1 in the “Test Your Understanding of Concepts and Principles” section located at the end of chapter 13 and let me guide you through one possible answer. Watch for key terms in boldface type, helpful tips and general suggestions on writing the essay or short‑answer questions. Enjoy!
114. Describe how the pacemaker cells produce a spontaneous diastolic depolarization, and how this leads to the production of action potentials.
Answer. During the resting period (diastole) of the heart, the fibers of the sinoatrial (SA) node region of the right atrium have unique channels that open in response to membrane hyperpolarization (approaching –60 mV) left over from the previous action potential. Since these channels are permeable to both Na+ and K+, the predominate entry of Na+ results in the net depolarization of these pacemaker cells producing spontaneous diastolic depolarization. Once threshold is reached, voltage-gated Ca2+ channels in the plasma membrane open resulting in the influx of Ca2+ that produces the upward phase of the action potential tracing and also results in contraction of these myocardial cells. After the spike, voltage-gated K+ channels open and the outward diffusion of K+ produces repolarization of the membranes that once again approach –60 mV with hyperpolarization that follows to repeat the cycle. The term “spontaneous” refers to the inherent property of myocardial pacemaker cells to beat automatically and on their own without the assistance of nerves or hormones. This property is known as automaticity.
OK, now that wasn’t so hard was it? Here are some more.
115. Draw and label two consecutive heart beats as recorded on the electrocardiogram (ECG). In sequence describe what occurs in the heart to create each electrical event. (Hint: This is a favorite test question!)
116. In three columns compare and contrast the structure and related functions of (a) arteries, (b) veins, and (c) lymph vessels. (Hint: Use a table format here, OK?)
117. Describe the first two events that occur when blood begins to clot starting from both the intrinsic pathway and the extrinsic pathway. State the important differences in these two pathways. Then, write the final two enzymatic steps in the formation of a fibrin clot (notice that these last steps are the same for both pathways).
118. Trace the recycling pathway of plasma fluid from capillary blood, through the extracellular (interstitial) spaces, its conversion to lymph fluid, and transport through lymph vessels to become part of blood once again. Name all structures involved and the forces (or pressures) that keep the fluids moving continuously. (Hint: Work slowly, this is difficult, but the result will give you an excellent overview of the lymphatic system.)
119. Describe the ABO blood typing system — including the genotypes responsible, the synthesis of A and B antigens from the DNA code, and the differences between the antibodies which are found in the plasma and the A and B antigens which are found on the red blood cell membrane.
Source: http://highered.mheducation.com/sites/dl/free/0072852933/221317/chapt13.doc
Web site to visit: http://highered.mheducation.com
Author of the text: not indicated on the source document of the above text
If you are the author of the text above and you not agree to share your knowledge for teaching, research, scholarship (for fair use as indicated in the United States copyrigh low) please send us an e-mail and we will remove your text quickly. Fair use is a limitation and exception to the exclusive right granted by copyright law to the author of a creative work. In United States copyright law, fair use is a doctrine that permits limited use of copyrighted material without acquiring permission from the rights holders. Examples of fair use include commentary, search engines, criticism, news reporting, research, teaching, library archiving and scholarship. It provides for the legal, unlicensed citation or incorporation of copyrighted material in another author's work under a four-factor balancing test. (source: http://en.wikipedia.org/wiki/Fair_use)
The information of medicine and health contained in the site are of a general nature and purpose which is purely informative and for this reason may not replace in any case, the council of a doctor or a qualified entity legally to the profession.
The following texts are the property of their respective authors and we thank them for giving us the opportunity to share for free to students, teachers and users of the Web their texts will used only for illustrative educational and scientific purposes only.
All the information in our site are given for nonprofit educational purposes
The information of medicine and health contained in the site are of a general nature and purpose which is purely informative and for this reason may not replace in any case, the council of a doctor or a qualified entity legally to the profession.
www.riassuntini.com